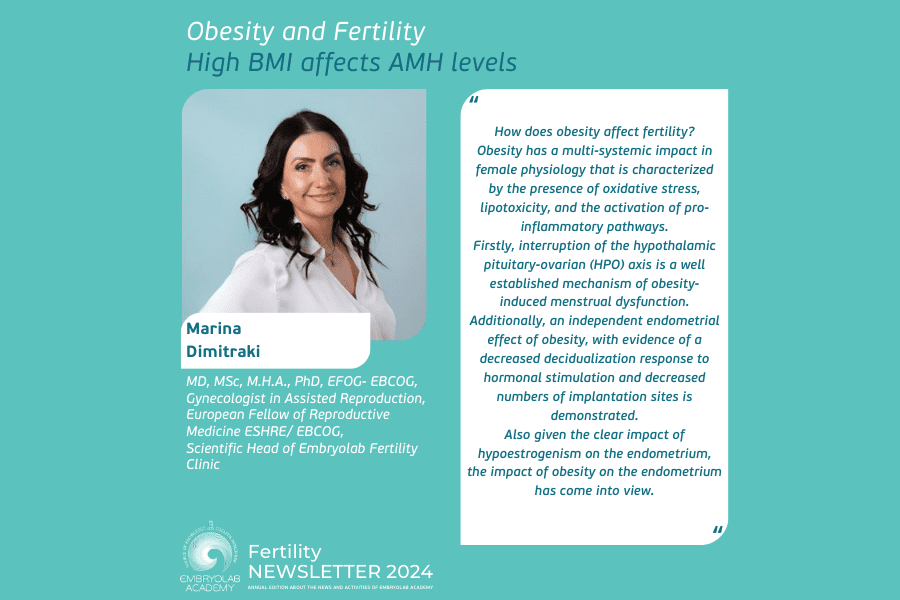
Marina Dimitraki, MD, MSc, M.H.A., PhD, EFOG- EBCOG, Gynecologist in Assisted Reproduction, European Fellow of Reproductive Medicine ESHRE/ EBCOG, Scientific Head of Embryolab Fertility Clinic
The prevalence of obesity worldwide is significantly higher in women than men. It is concerning specifically in women of reproductive age, as it is critical for them not only to address the general health risks of obesity, but also to consider the impact of obesity on reproductive health. Obesity has been linked to lower spontaneous pregnancy rates and has also been associated with poorer outcomes in women undergoing in vitro fertilization (IVF).
How does obesity affect fertility? Obesity has a multi-systemic impact in female physiology that is characterized by the presence of oxidative stress, lipotoxicity, and the activation of pro-inflammatory pathways.
Firstly, interruption of the hypothalamic-pituitary-ovarian (HPO) axis is a well-established mechanism of obesity-induced menstrual dysfunction. Additionally, an independent endometrial effect of obesity, with evidence of a decreased decidualization response to hormonal stimulation and decreased numbers of implantation sites is demonstrated. Also given the clear impact of hypoestrogenism on the endometrium, the impact of obesity on the endometrium has come into view.
Moreover, it is of great interest obesity has a direct effect on the ovary and oocyte. Human studies demonstrate morphological oocyte abnormalities and decreased oocyte competence with obesity. It is of great importance that BMI seems to be associated with serum AMH levels. Several recent large-scale studies demonstrated significantly lower AMH levels among women with increased BMI with and without PCOS. In other studies, obesity on the basis of either percent body fat or BMI was associated with lower serum AMH levels. AMH concentrations were 23.7% lower and antral follicle count decreased in women with obesity compared with women with normal weight.
Concerning the field of in vitro fertilization (IVF), women who have a higher body mass index (BMI) have decreased responses to fertility medications, fewer oocytes retrieved, and lower pregnancy and live birth rates than those who have a normal BMI.
Specifically, oocytes from females with obesity undergoing are often smaller compared with their normal weight counterparts. are less likely to complete development postfertilization, and resulting blastocysts demonstrate altered metabolism, with reduced glucose consumption and increased levels of triglycerides. In addition, obesity is associated with meiotic spindle abnormalities and fewer mature oocytes. Moreover, the follicular fluid of females with obesity demonstrates significantly altered adipokine composition, inflammatory markers (C-reactive protein), and free fatty acids (67– 70). The increased systemic leptin present with obesity is similarly evident in the follicular fluid of women with obesity, who have higher levels of intrafollicular leptin compared with women of normal weight. Leptin has been also shown to directly suppress both antimullerian hormone (AMH).
Data suggest a possible cumulative effect of obesity: women with obesity present since age 18 years had AMH levels that were significantly lower than women with normal weight at age 18 years but who currently had obesity. Although diet reversal improves the circulating metabolic milieu, meiotic and mitochondrial abnormalities persist, suggesting that obesity may induce an irreversible insult to the ovary.
REFERENCES
Lia A. Bernardi, Mercedes R. Carnethon, Peter J. de Chavez, Deborah E. Ikhena, Lisa M. Neff, Donna D. Baird, Erica E. Marsh, Relationship between obesity and anti-Müllerian hormone in reproductive-aged African American women, Obesity 2017,Volume25, Issue1,P 229-235
Samantha B. Schon,Hannah E. Cabre,Leanne M. Redman, The impact of obesity on reproductive health and metabolism in reproductive-age females, Fertility and Sterility 2024, Volume 122,Issue 2p193-394.
Julie S. Rhee, Jessica L. Saben, Allyson L. Mayer, Maureen B. Schulte, Zeenat Asghar, Claire Stephens, Maggie M.-Y. Chi, Kelle H. Moley,
Diet-induced obesity impairs endometrial stromal cell decidualization: a potential role for impaired autophagy,Human Reproduction, 2016, Volume 31, Issue 6, 1315–1326
Oldfield AL, Kazemi M, Lujan ME. Impact of obesity on anti-mullerian hor- mone (AMH) levels in women of reproductive age. J Clin Med 2021;10: 3192
Jaswa EG, Rios JS, Cedars MI, Santoro NF, Pavone MEG, Legro RS, et al. Increased body mass index is associated with a nondilutional reduction in antimullerian hormone. J Clin Endocrinol Metab 2020;105:3234–42
Leary C, Leese HJ, Sturmey RG. Human embryos from overweight and obese women display phenotypic and metabolic abnormalities. Hum Re- prod 2015;30:122
Gonzalez MB, Robker RL, Rose RD. Obesity and oocyte quality: significant implications for ART and emerging mechanistic insights. Biol Reprod 2022; 106:338–50
Gonzalez MB, Lane M, Knight EJ, Robker RL. Inflammatory markers in hu- man follicular fluid correlate with lipid levels and body mass index. J Reprod Immunol 2018;130:25–9.