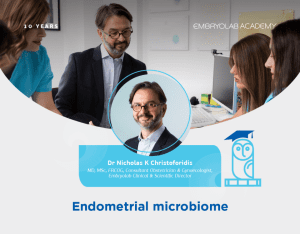
Dr Nicholas K Christoforidis, MD, MSc, FRCOG, Consultant Obstetrician & Gynaecologist, Embryolab Clinical & Scientific Director
Dr Nicholas K Christoforidis, MD, MSc, FRCOG, Consultant Obstetrician & Gynaecologist, Embryolab Clinical & Scientific Director
Does the endometrial cavity have a unique molecular microbial signature?
A starting point in the discussion of the endometrial microbiome is its origin. How do micro-organisms reach the endometrial cavity? It seems likely that there are more than one possible routes of colonisation, with the ascending vaginal route being the commonest. There is good evidence that the uterus through its peristaltic contractions works as a naturally occurring pump, facilitating entrance of bacteria from the vagina and through the cervix. But apart from the ascending route, colonization can be blood-borne, while microbes can reach the endometrial cavity even through ART procedures, mainly embryotransfer and oocyte pick-up.
Many studies have investigated the composition of endometrial microbiota, usually in the context of infertility research. So far, no consensus has been reached on the profile of either a normal endometrial microbiome, or the characterisation of bacterial pathogens and the mechanisms by which they could interfere with embryo implantation.
However, there is a certain body of literature that supports the abundance of Lactobacillus species as the principle micro-organism of a normal endometrial microbiota. A good number of studies have associated the presence of lactobacilli with reproductive outcomes in ART treatment, while depletion of lactobacillus in endometrial microbiota has been shown to result in dysbiosis and pathological growth of bacteria associated with gynaecological pathology, such as infertility, miscarriage, preterm birth and gynaecological malignancy.
Lactobacillus-dominant microbiota favours reproductive function, through a wide range of actions which aim to prevent bacterial colonisation by pathological bacteria. Evidence from research on the vaginal lactobacilli shows that pathogens are successfully kept away through lactobacillus production of hydrogen peroxide and antibacterial substances, as well as through competitive adhesion to epithelial cells.
On the other hand, not all researchers agree that lactobacilli constitute the basis of a healthy endometrial microbiota, with sampling contamination through the vagina and cervix being a valid argument in support of their stand. Actually, when direct sampling from the endometrial cavity is performed in order to minimise the risk of transcervical contamination results appear quite different. As in the study by Winters et al, when sampling the endometrium of hysterectomised women for benign pathologies they concluded that the dominant bacteria isolated included Acinetobacter and Pseudomonas, while the presence of Lactobacilli was rare.
Does a healthy microbiota stay the same or it varies and if so, which factors can account for the variations observed?
A healthy endometrial microbiome appears to change both short and long term in women. Female age is a recognised factor associated with variation in microbiota, with older women presenting smaller differentiation and variation in their own microbial populations, while on the other hand differentiation and variation may increase in between women as they age. Variations are also observed during the menstrual cycle. The lactobacillus population is significantly decreased just after the start of menses, only to start gradually increasing in numbers during the follicular phase, reaching a peak during the luteal phase.
What is the role of a healthy microbiome with regards to endometrial function?
So far, it has become clear from previous studies and other disciplines in medicine that microbiota and mammals depend on their symbiotic relationship. While microbes receive a steady nutrient supply through the host, the host benefits from vital contributions of the microbe to physiological processes such as epithelial homeostasis. Commensals provide a natural barrier against colonisation by pathogenic species and ensure optimal epithelial function.
What happens when the endometrial microbiota is disturbed resulting in dysbiosis?
A local inflammatory response is triggered with immunocompetent B cell lymphocytes differentiating into plasmacytes capable of producing a variety of Ig subclasses against specific antigens of pathogens. Chronic endometritis is commonly the result of dysbiosis of the endometrial microbiome.
Chronic endometritis is a persistent inflammation of the endometrial mucosa caused by bacterial pathogens such as Enterobacteriaceae, Enterococcus, Streptococcus, Staphylococcus, Mycoplasma, and Ureaplasma. Although chronic endometritis can be asymptomatic, it is found in up to 40% of infertile patients and is responsible for repeated implantation failure and recurrent miscarriage. Diagnosis of chronic endometritis is based on hysteroscopy of the uterine cavity, endometrial biopsy with plasma cells being identified histologically, while specific treatment is determined based on microbial culture. However, not all microorganisms implicated are easily or readily culturable needing a turnaround time of up to 1 week.
The group of I. Moreno and colleagues have looked into the application of real-time PCR for the identification of 9 chronic endometritis pathogens and compared it sensitivity to hysteroscopy and histology with staining of the endometrium, concluding that molecular techniques, such as RT-PCR and NGS allow for identification of culturable and non-culturable endometrial pathogens with a high degree of concordance with all other diagnostic methods, providing an opportunity to improve the clinical management of infertile patients with such an endometrial pathology.
What about the association of the endometrial microbiota and reproductive outcomes in ART?
A number of studies have looked into the impact of endometrial microbiome and chance of pregnancy following IVF, with often conflicting results. Most studies were done with NGS techniques, while sampling of the endometrium in the majority was done from the catheter tip, or through endometrial fluid aspiration.
The group of Inmaculada Moreno from Spain consistently showed that lactobacillus-dominant communities where clearly associated with improved reproductive outcomes following IVF treatment, especially when the percentage of lactobacilli was over 80-90%.
Lately, the same group, published a multi centre prospective observational study using NGS to analyse endometrial fluid and biopsy samples before ET in a cohort of 342 infertile patients, asymptomatic for infection undergoing ART. Lactobacillus was consistently more abundant than dysbiotic or pathogenic bacteria in women that achieved a pregnancy
In addition, absence of bacteria, including Lactobacillus was not a forbidding factor for implantation, reinforcing the evidence supporting the role of pathogenic bacteria as a risk factor in reproduction.
So, if dysbiosis is associated with poorer reproductive outcomes we should be aiming to restore a normal microbiota. Many studies have confirmed the effectiveness the of broad-spectrum antibiotics in combination with probiotics in this context. The benefit of antibiotic treatment for chronic endometritis in infertile patients appears quite clear, especially these diagnosed with recurrent implantation failure.
We should note that a significant limiting factor in current methods of endometrial microbiota assessment is sample contamination, either cross-contamination from the vagina and cervix, or due to poor characterisation of contamination controls. To this we should note the lack of healthy controls. All these may lead to misinterpretation of a low-abundance site, without being always in a position to judge whether microbes isolated are true residents, or pathogens.
With regards to the molecular techniques, and in specific NGS, it should be noted that the current method based on 16s rRNA gene V region variation may over or under present certain microbial taxa and that there is a need to standardise methodology in taxonomic unit classification.
Moreover, NGS does not represent viability, it only quantifies 16s rRNA gene, so in reality positive results may represent equally a past infection, not necessarily an active condition.