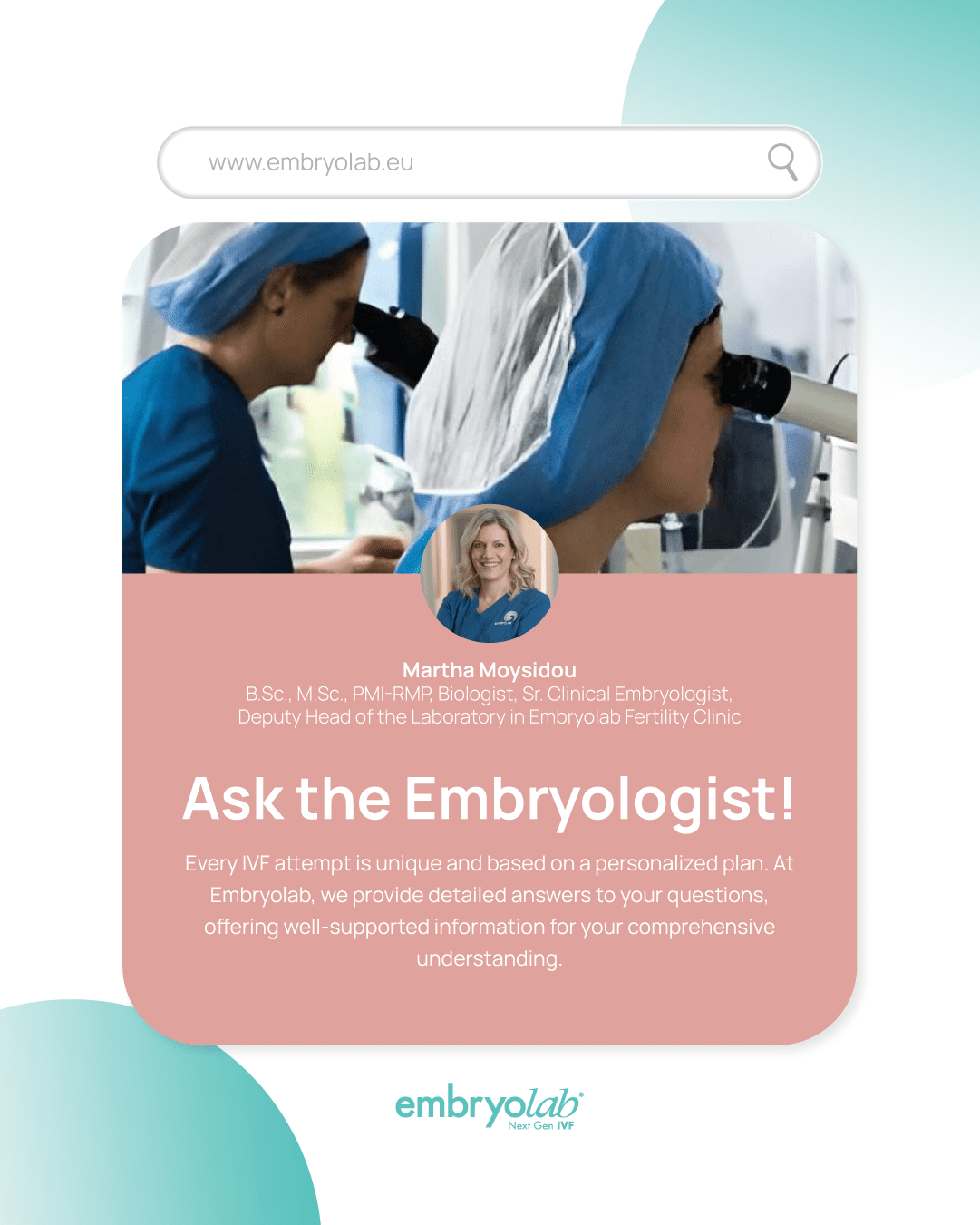
Martha Moisidou, BSc, MSc, PMI-RMP, Senior Clinical Embryologist, ESHRE certified, Lab Deputy Director, Lab Quality Control Manager
You ask — the Clinical Embryologist answers!
The treatment plan designed for each couple undergoing in vitro fertilization (IVF) is unique and fully personalized. From sperm processing and management to embryo selection for transfer, the laboratory strategy is a key element of success.
For this reason, a fundamental priority for all of us at Embryolab is ensuring that patients have direct access to the embryology team. Clinical embryologists are able to evaluate the male partner’s test results (sperm analysis and additional sperm tests), as well as the couple’s previous embryological history. This allows them to make the necessary laboratory decisions aimed at achieving the best possible outcome.
- Sperm processing: which innovative methods improve prognosis?
Beyond the classic semen analysis—which determines sperm concentration, motility, and morphology—innovative tests such as DFI, FISH, and oxidative stress measurement shed light on additional sperm parameters.
Identifying any pathology is crucial, as it determines the man’s preparation (vitamin supplementation, ejaculation frequency) and, most importantly, the method used to process the sample during fertilization.
We now have access to microfluidic sperm sorting devices, which isolate sperm with the highest possible DNA integrity. By using these selected sperm cells, we create a stronger foundation for the new life developing in our laboratories, significantly improving prognosis.
- Embryo morphology: how does it affect developmental potential?
The morphology of an embryo and how it influences its implantation potential is a subject that concerns both reproductive specialists and couples alike.
Years of research have led to a deeper understanding of the preimplantation embryo needs and to improvements in culture conditions. This allows each embryo to reach its maximum developmental potential.
The experience of clinical embryologists, combined with technological expertise—such as optimized culture media, time-lapse incubators, and assisted oocyte activation—leads to optimal embryo morphology and, ultimately, successful outcomes.
- Use of time-lapse incubators (e.g., EmbryoScope) and artificial intelligence: what are the advantages?
New-generation time-lapse incubators offer a unique advantage in monitoring embryo development: they allow continuous observation of embryos without exposing them to external environmental conditions.
These incubators are nowadays equipped with integrated AI applications, which enhance embryo evaluation even further. This enables reproductive biologists to perform a more detailed ranking of embryos, as subtle developmental differences can reveal the most viable one—reducing the time to pregnancy!
- Preimplantation Genetic Testing for Aneuploidies (PGT-A): who benefits?
PGT-A is recommended for couples or women who have an increased likelihood of chromosomal abnormalities in their embryos (e.g., advanced maternal age, abnormal parental karyotypes) or those who have experienced recurrent miscarriages.
The technique involves performing a biopsy on the embryo to isolate a small cluster of cells, which are then analyzed in a specialized genetics laboratory. The results reveal which embryos have a normal chromosomal constitution and therefore the potential to result in a healthy child.
This diagnostic tool requires careful consideration: on one hand, it provides valuable information about whether an embryo should be used; on the other, the biopsy removes a small amount of cellular material, which—even minimally—might affect the embryo’s developmental potential.
At Embryolab, we present each couple or woman with the embryological data, discuss it thoroughly, and recommend whether or not to proceed with PGT-A, depending on the number of available embryos, their morphology, and the reasons behind considering this option. In every case, the potential benefit of the procedure must outweigh any possible impact on the embryos.
- Embryo transfer: how does the clinical embryologist select the embryos?
Selecting embryos for transfer—whether in fresh or frozen cycles—is the culmination of an IVF process. Timely and accurate embryo selection maximizes the chances of pregnancy.
An algorithm is formed by assessing multiple factors: the embryo’s developmental progress in the incubator, the timing of cell divisions, the percentage of cell fragmentation, its final morphology, and the clinical embryologist’s expertise.
When embryos have very similar characteristics, AI applications provide an additional tool to help select the embryo(s) with the best prognosis.
In frozen cycles, the ranking and cryopreservation of embryos are performed in a similar manner, ensuring that each cryostorage unit includes the full developmental history of the embryo it contains. This guarantees precise and targeted thawing and use of each embryo.
The development of technology and the use of all innovative tools, now available, enable assisted reproduction specialists to offer improved embryological outcomes. Tailoring these applications to the specific needs of each couple or woman, ensures the best possible conditions on the path to parenthood.